How video games can strengthen the relationships seniors value most
While the vast majority of video gaming enthusiasts are millennials, a growing crop of older adults are accessing video gaming technology for entertainment, cognitive stimulation, physical activity, and social fulfillment. They’re even making video games a part of their health and well being.
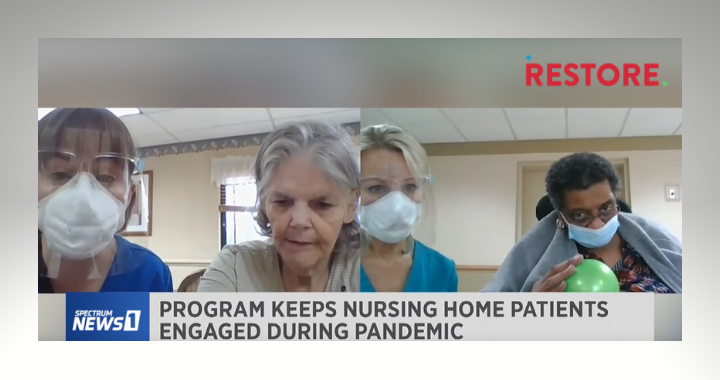
During the pandemic, the increased adoption of video games among seniors is proving to be more important than ever. This is especially true for skilled nursing and senior living residents in need of a lifeline to counter the effects of social isolation and loneliness.
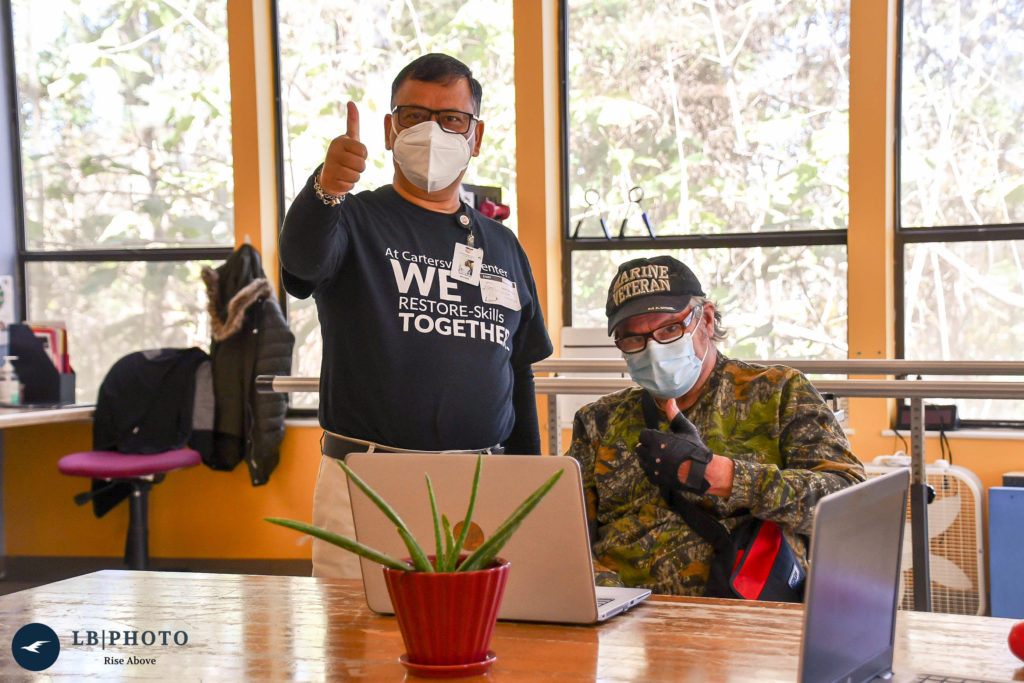
Some senior care centers are even using video games as a means of skill-building, applying newly developed therapy and wellness technologies into their clinical approach. In my work as CCO and occupational therapist at RESTORE-Skills, I regularly see seniors use gaming technology to reach therapy milestones faster and improve physical and cognitive abilities. At the same time, they’re strengthening relationships with loved ones and friends by connecting virtually via fun, therapeutic video games on our platform. This happens all from the safety of their rooms.
All of this comes as no surprise to those studying the impact of video games on seniors. A study of adults ages 60-80 published recently in Behavioural Brain Research indicated that video games may be used to enhance cognitive health in older adults. The findings suggest that both novel experiences and exposure to rich three-dimensional environments may work together to improve cognition.
Based on these findings and my own experience, skilled nursing facilities and senior living communities need to become early adopters of this new technology or be left behind.

Tournament gaming enhances social connections and fosters a sense of community
Users of RESTORE-Skills also benefit socially and emotionally by playing virtual tournaments against friends and family as part of their therapy and wellness regiment. What’s more, they’re sharing a common language with Millennial and Gen Z grandchildren outside of these sessions.
This is because there can be limits to conversation among seniors and their loved ones, especially for those in skilled nursing homes dealing with language impairments. It doesn’t help that many younger people are accustomed to rarely making phone calls, preferring text and social media apps instead.
The wider the generation gap, the harder it is today to make small talk.
Unless you’re talking about video games.
Skilled nursing and senior living residents learn a new language to share with younger relatives
Consider the following example from among skilled nursing patients we have served in therapy. A male patient, and former salesman with a gift for gab, suffered a stroke and had expressive aphasia, limiting his ability to communicate. He also had limited movement of his right upper and lower extremities. When we introduced him to our therapy video game solution, he was eager to give it a try. Although he had never played video games before, he considered it a way to impress and relate to his son and grandson, both avid video game players.
This patient is one of many.

A study published in Sage Journals revealed that sharing in video games fosters relationships and connections while producing positive emotions for both grandparents and grandchildren. “As a consequence, game designers should take into consideration ways to enhance these social aspects of gameplay.”
Seniors who play video games now have a shared language to connect with their kids or grandkids. Instead of brief conversations about what’s happening at school, they can instead play a game together and make it part of the patient’s therapy exercises.
Prior to the pandemic, one 88-year old senior living resident and great-grandmother was introduced to a virtual skill-building therapy session to improve her range of motion, coordination, and ability to perform activities of daily living. She willingly participated but wasn’t overly enthusiastic.
Ten minutes into the session, her two great-grandsons surprised her with a visit, raced into the room and asked for a turn. She shared her red ball-shaped controller, and the boys took turns sitting on her lap while they waited to play.
The staff later learned this was the first time one of the boys, who has autism, had ever entered his grandma’s room willingly and engaged physically. Such is the potential healing and connective power of this essential language and activity.
This kind of interaction makes a difference in any scenario, but especially in a season where grandkids are holding up signs at windows of skilled nursing facilities in lieu of actual visits.
Video games create generational connection while providing crucial therapy
Learning the language of video gaming gives both family members and their senior relatives a productive way to spend time together. And, the pandemic has led more seniors to be open to adopting new technology out of pure necessity.
In 2020, the pandemic propelled the video game industry to make more money than movies and North American sports combined. There’s no indication this will slow in 2021.
As more people adopt video gaming technology, the benefits are clear. Research is showing the power of video gaming, especially on cognition of older adults; making it crucial that video games are widely adopted by healthcare.
Adding therapy to video games and enabling families to connect through the technology is an incredible opportunity for post-acute rehab providers especially.

Making therapy fun with video games leads to better outcomes
Refusals are always a challenge for healthcare professionals to overcome, especially in skilled nursing and rehab facilities. However, making therapy and wellness sessions fun and engaging can lead to more positive outcomes.
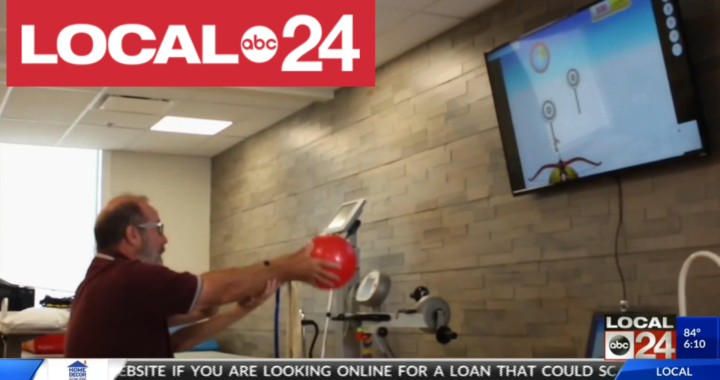
One male patient who had a history of multiple falls and therefore a reluctance to leave his room was refusing physical therapy support. However, he eagerly agreed to try out the RESTORE-Skills video gaming platform as a fun way to achieve his balance goals and reduce his risk of falling.
He was able to virtually ski in a world cup race, pull a slot machine handle to win a jackpot, and rock climb to the top of an ancient temple – all interests he had never experienced before. As soon as he finished his session, he shared how excited he was to tell his grandson all about his experience. He actually remained in the therapy clinic to watch and encourage others as they participated.
Making video gaming accessible for seniors
The key to successfully adopting video gaming technology for those in senior care centers is making the video games accessible and user friendly. Any video gaming technology for seniors must have the following features:
- Easy to access
- Easy to learn
- Easy to use
- Gradable (adaptable to an individual’s abilities)
- Relatable
- Meaningful
- Have audio and video call compatibility
Access to virtual communities of friends and peers
Besides making therapy fun, video games inspire users to play and achieve more through gamification. Competition, collaboration, achievements, and a sense of community drive people to meet their goals in an enjoyable way.
Our RESTORE-Together feature allows patients and players to play interactively with loved ones and friends in a facility or across the country from the safety of their rooms. One patient’s siblings were unable to visit during a recent short-term rehabilitation admission. They worried that their phone calls didn’t provide enough meaningful connection.
The healthcare team coordinated for the patient’s siblings to join his therapy session to encourage him and participate themselves. They watched their brother stand for ten minutes at a “slot machine,” trying to win the jackpot with a weighted controller. It was a huge improvement over his previous best record of only one minute.
The therapist was then able to send a code to the patient’s siblings so they could play a slot machine tournament together, followed by a “Let it Snow Bingo” game that helped with hand-eye coordination, sustained attention, strengthening, and activity tolerance.
Being able to share this experience with others is a key to healing success.

The fact that seniors can use video games to connect to their loved ones is an added bonus to the physical, cognitive, and psychosocial benefits the technology offers. The gamification and fun aspects make programs like RESTORE-Skills appealing enough for seniors to work on skills more effectively.
Confidence to strengthen the mind, body, and social connections that matter most
When seniors have access to video game technology for skill-building, they experience greater confidence, as well as an increased desire to regain social skills and connections. Even the staff enjoys training and learning how to use this technology to benefit their patients.
Video games are most successful when they are easy to access, easy to learn, and easy to use. The game must also be gradable, or adaptable to an individual’s ability. The more relatable and meaningful the games are to the individual, the more the patient is excited to use the program.
Skilled nursing facilities and senior living communities must adapt to offer residents the opportunity to learn the language of video games. By creating virtual communities, tournaments, avatars, and immersive experiences in a world without borders, seniors can work on developing skills in a meaningful, collaborative and entertaining way.
Just don’t be surprised when grandma gets the high score!