Question:
How can we use RESTORE in the delivery of group and concurrent therapy?
Answer:
Great question. To start we have to understand the difference between group and concurrent therapy:
- Group Therapy - One therapist/asst. providing treatment of 2-6 patients performing similar functional skill activities that are part of their plans of care regardless of payor source.
- Concurrent Therapy - One therapist/assist. providing treatment to 2 patients simultaneously, who are performing different functional skill activities (per payor guidelines).
Next, let’s look at some of the potential benefits of these deliveries of care approaches:
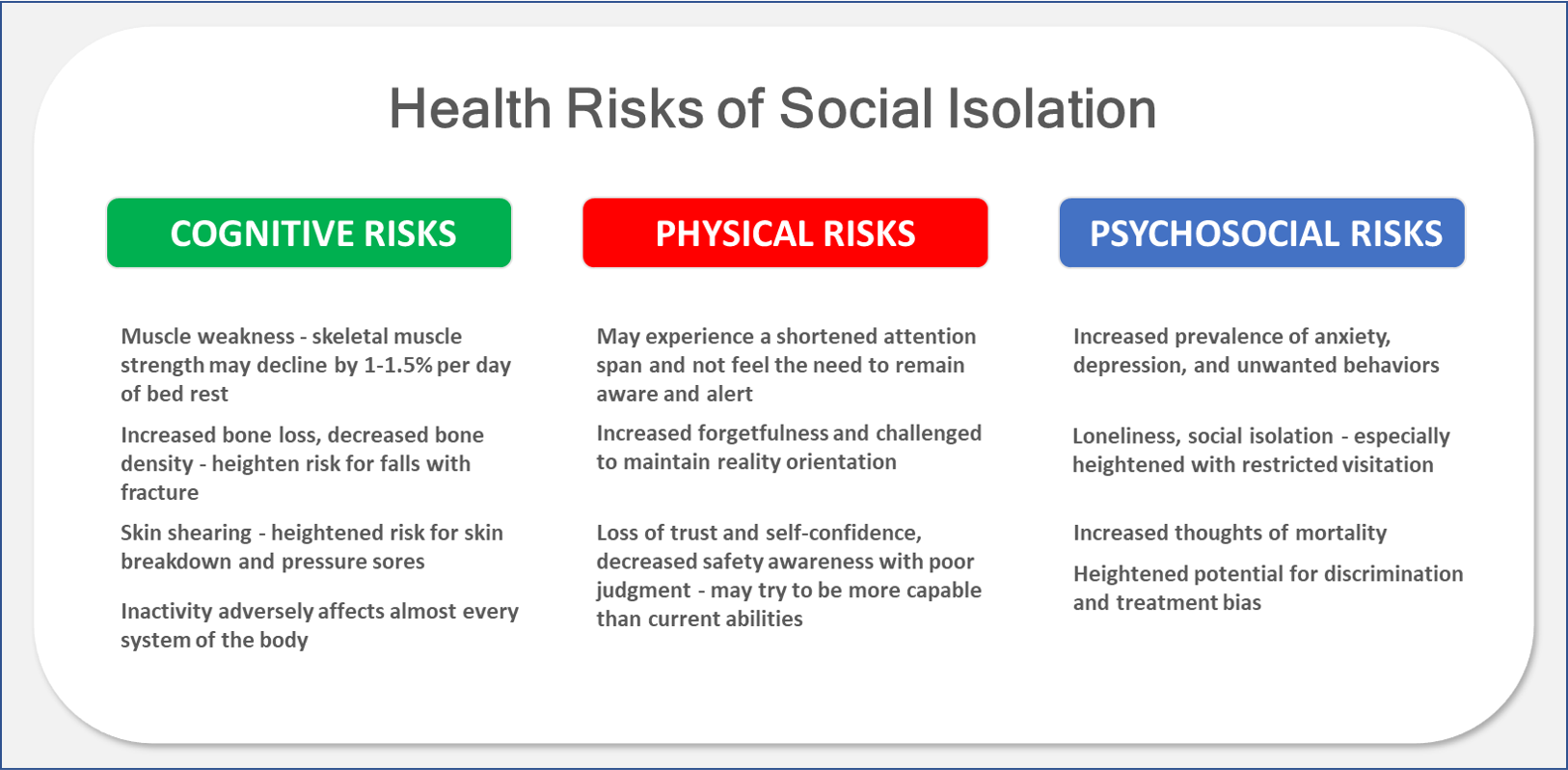
- Socialization - helps mitigate the risks of isolation/loneliness and promotes social interaction skills.
- Patterning of Behavior - promotes the ability to learn from others. Players of similar or different functional ability levels can benefit from observing/demonstrating how to perform an activity that helps to improve their own performance outcomes.
- Cooperation - the ability to work together towards a common goal can be rewarding and motivating. By working together, players can achieve outcomes they may never have realized individually.
- Competition - many players are motivated by competition. They may in fact participate longer, move more, and engage more when there is an opportunity for a winning outcome.
- FUN - the most important benefit is that skill-building with others is more enjoyable than skill-building alone.

RESTORE can be used in support of both group and concurrent therapy
Progress can be accelerated by combining socialization, patterning of behavior, and functional skill-building with immersive, interactive content (preferably person-centered based on the expressed interests of each player). Let’s consider the following:
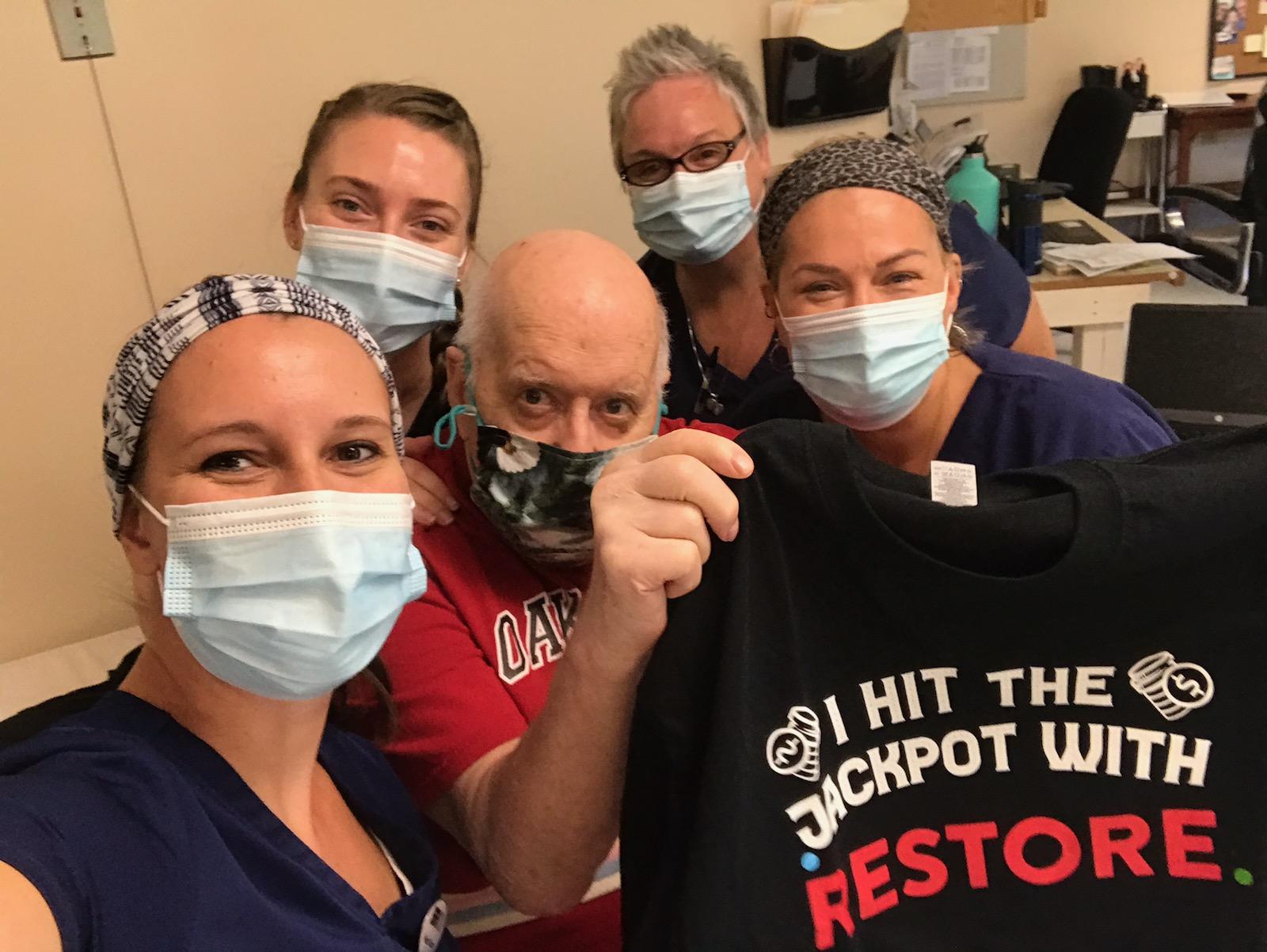
- 2-6 patients (players) who share a common interest, such as casino gaming, and have therapy plan of care goals to increase activity tolerance (sitting or standing), upper extremity range of motion, coordination, and sustained attention would enjoy participating in a Jackpot, Plinko, or Bingo competition. Players can be in the same room and remain socially distanced while set up with a device with a webcam (laptop, tablet, iPad) and simultaneously address functional skills while performing a friendly competition or just trying to achieve personal bests. Players are able to encourage one another through social interaction, while additionally patterning behavior from other players to help them better achieve their personal desired skill-building outcomes.
- 2 players who may or may not share a common interest can each be set up with a device and the therapist can facilitate concurrent activities addressing desired functional skill-building with both players. A therapist may also choose to have both players participating on the same screen at the same time while working on different functional skills. For example, one player may be pulling the handle of a slot machine on the right side with his/her upper extremity while sitting and a second player may be pulling the handle on the opposite side of the slot machine with a squat or lower extremity while standing. Although the enjoyment of the same game is appreciated, each player is working on distinctly different functional skills concurrently.
Set up & selection options for the delivery of group and concurrent therapy
-
Group Play
- Scoring is recorded on a leaderboard. Players can attempt to beat their personal best score and even make their mark on the All-Time Leaderboard
- 2 Players - Cooperative
- Best for grouping two players playing at the same time on the same screen requiring similar functional skill-building
- Concurrent consideration in this mode is to have 2 players on the same screen at the same time requiring different functional skill-building
- 2 Players - Taking Turns
- Best for grouping two players, taking turns to encourage each other, pattern behavior, and facilitate competitive motivation
- More than 2 Players - Taking Turns
- Best for grouping more than two players, taking turns to encourage each other, pattern behavior, and facilitate competitive motivation
-
RESTORE Together
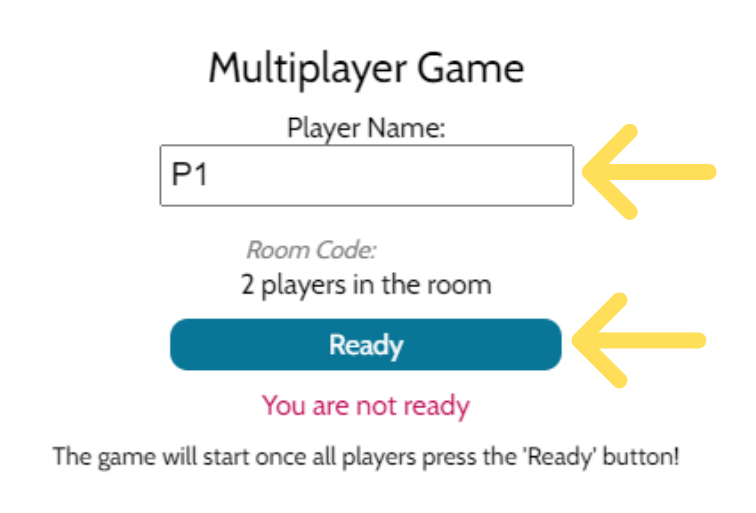
- Players from different devices compete in the same game, same setting competition to see who can achieve the top score.
- Private Game
- Best for facilitating a group of 2 or more players in the same location on different devices who desire to experience interactive game play. Players compete with our default settings in a competition where players are able to see their place (who is in first, second, third, etc.) and scoring outcomes in real time
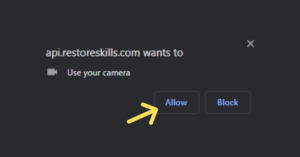
- A therapist will create a private game on one device and assist players on different devices to access the private game via a unique code that is entered at app.restoreskills.com/together
-
Single Game
- Best for group treatment with the therapist providing each player a device and:
-
- Addressing the same functional skill-building with different games or individualized settings for the same games
-
- Best for concurrent treatment with the therapist providing each player a device and:
-
- Addressing different functional skill-building with different games or the same game but working on a different functional skill
-
- Best for group treatment with the therapist providing each player a device and:
-
Tournament Play
-
- This is created by the RESTORE team upon request. Play can be enhanced with the creation of a "same game" tournament or multi-game Olympic event-style competition. Events can occur within one location or across multiple locations simultaneously. An event can be created as a single day or multi-day event.
When players (patients) are having fun and engaged they focus less on targeted skills and more on the game. They have less anxiety or frustration when able to experience success, learn from one another, and feel a sense of accomplishment. Therapists are able to appropriately incorporate functional skill-building groups or concurrent treatment using RESTORE for more effective and efficient outcomes.