By Ian Oppel, CCO of RESTORE, occupational therapist, and 20-year Dementia Capable Certified Therapist
While residents in skilled nursing facilities continue to struggle in the fourth month of this new normal, those with Alzheimer's disease and dementia have the added challenge of communication barriers, decreased engagement, and the struggle to maintain cognitive function now even more. These are people who depend on a familiar routine, secure connections with loved ones, and group activities to slow the progression of a cruel disease.
In honor of this June's Alzheimer's and Brain Awareness Month, I want to raise awareness of how RESTORE's interactive gaming therapy software is key to supporting long term care's most vulnerable residents.
Those at the highest risk for deterioration of the disease process with COVID-19 are dementia patients.
Individuals with dementia function best with routine. They need the familiarity of a caregiver and a consistent environment. But because of COVID-19, regular routines are completely disrupted. Like everyone in skilled nursing facilities, those with dementia are spending most of the day in their rooms, often alone and isolated. They aren't able to socialize in group activities and with loved ones, which usually keeps them engaged and able to pattern behavior after others.
The goal when working with individuals living with Alzheimer's and dementia is to promote their best ability to function to slow or delay the deterioration of a progressive disease. It starts with gaining agreement, followed by making changes to the environment, activity, and/or care partner approach. After working with this population, I know firsthand this takes time and patience because helping residents with Alzheimer's can be so much faster than supporting them to be independent. It's a good intention to want to jump in and help, but supporting these residents too much can leave them more helpless. This is a challenge always, but no doubt, it's even harder now that facilities are staffing challenged.
This is why I consider RESTORE the perfect medium to slow the progression of memory care patients. I've seen patients find engaging games connected to their life history, interests, and abilities. The games support cognitive and behavioral skills, and of course, physical skills.
Take the WWII pilot I met at our client's facility before COVID-19 hit. He didn't want to work on the motion of lifting his arm to reach for a cone; his therapist was extending in front of him. When I learned that he was a pilot in World War II, I offered to show him our Take Flight game. He ended up getting really engaged and even told me the highlight of his life was meeting General Patton. By the end of our session, he had held his arm and sustained action several times for over two-minute intervals, something that's hard even for me but necessary for completing activities of daily living. And this is just one example of so many.
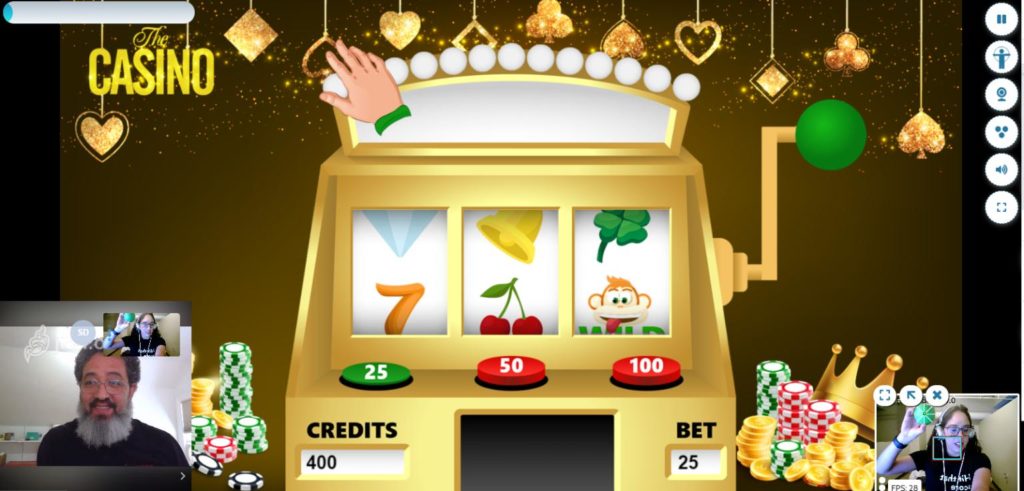
I'm seeing therapists and even activities staff customize RESTORE to support patients' cognitive and physical abilities, as well as their interests, preferences, habits, tendencies, professions, and family history. Players can golf, pull a slot machine lever, ski in a race, or fly a plane. RESTORE's 30+ games keep players engaged, as well as help with issues such as attention span, concentration, problem-solving, decision-making, and sequencing. Every game exercises cognitive functioning, helping patients with dementia to maintain attention, concentrate, and tap into procedural, working, and long term memory centers.
Add to this personalization feature the fact that RESTORE is portable and works on any device with a webcam. It's easy to set up and allows every staff member to support skill-building therapy. It's one thing to bring a dementia patient an iPad to play a sensory game or call a family member, but how much more impactful is software that lets patients actively play without handling a device, get immersed in the activity, and invite loved ones to participate virtually?
Connect to family and friends
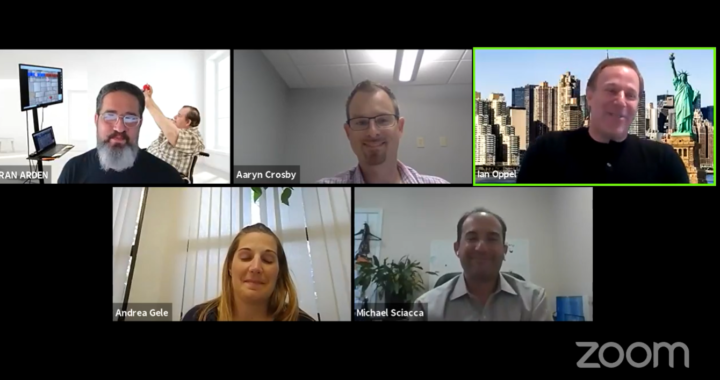
Just as COVID-19 hit, we added a feature to invite loved ones to join therapy sessions virtually. Having family interaction takes engagement to a whole different level. This is something that we just really haven't ever had the ability to do as therapists. It's incredible to share active treatment sessions with family members who can offer support, encouragement, and help build trust.
While family members are not able to come to the facilities these days, RESTORE can connect family members from where they are and bring them into the room virtually. Once you gain a patient's trust, now they can play RESTORE and have their family members come up on the screen and be able to interact.
If the family video is too distracting, we can always hide their video, and players can continue with just their loved one's voices.
I hear clients' stories every day of how RESTORE is keeping residents happy, active, and engaged during this new normal. It's keeping them connected to their families and able to do meaningful therapy work together with their loved ones' support. And for Alzheimer's and dementia patients, who are the most at risk right now, RESTORE is helping to slow down deterioration even amid the COVID-19 pandemic.